Psycho-neuro-endocrino-immunology (PNEI)
PNEI or the neuro-endocrine-metabolism (NEM) approach promotes understanding of the interconnection and communication between these self-regulating systems. Metabolism is seen here in a broad sense, covering immune, detoxification and energy production systems.
These control systems are both complex and interrelated, to the extent that an action on one system will have a positive or negative consequence on the others.
If we start from a problem of adrenal fatigue – which is often the starting point with problems of the gastrointestinal/microbiota system – we can better understand its impact on the other glandular systems: pancreas, thyroid, gonads (ovaries and testes).
Adrenal fatigue and thyroid hypofunction
Adrenal fatigue, for example, can trigger hypothyroidism and aggravate existing primary hypothyroidism. The symptoms of secondary hypothyroidism are very similar, if not identical, and result from poor thyroid function caused by dysfunction of another organ system.
Adrenal fatigue is perhaps the most common cause of secondary hypothyroidism, both clinically and subclinically. Low adrenal function often leads to low thyroid function, classically manifested by low free T4, low free T3, high TSH and low body temperature. Fortunately, secondary hypothyroidism can be reversed when the underlying problem (such as adrenal fatigue) is resolved.
When the adrenals are exhausted, their ability to manage the stress associated with normal bodily functions and energy requirements is often compromised. To promote survival, the adrenals force down-regulation of energy production. In other words, the body undergoes down-regulation of metabolism to slow down in order to conserve energy. The body needs to rest. Lower energy production reduces the body’s workload.
Symptoms of hypothyroidism:
- I feel tired and lethargic
- Cold hands and feet
- I need a lot of sleep to function
- I gain weight even if I eat little or on a low-calorie diet
- I suffer from slow intestinal transit and constipation
- I experience depression and lack of motivation
- I have morning headaches that disappear as the day progresses
- My hair and eyebrows are thin and fragile
- Dry skin and scalp
Adrenal fatigue and hypoglycemia
In the case of adrenal fatigue, symptoms of hypoglycemia are most often subclinical. This means that the person presents symptoms of clinical hypoglycemia even though blood glucose levels are invariably above 3.3 mmol/l. Their fasting blood glucose and glucose tolerance tests are usually normal. Conventional physicians unfamiliar with the influence of the adrenals will miss the point.
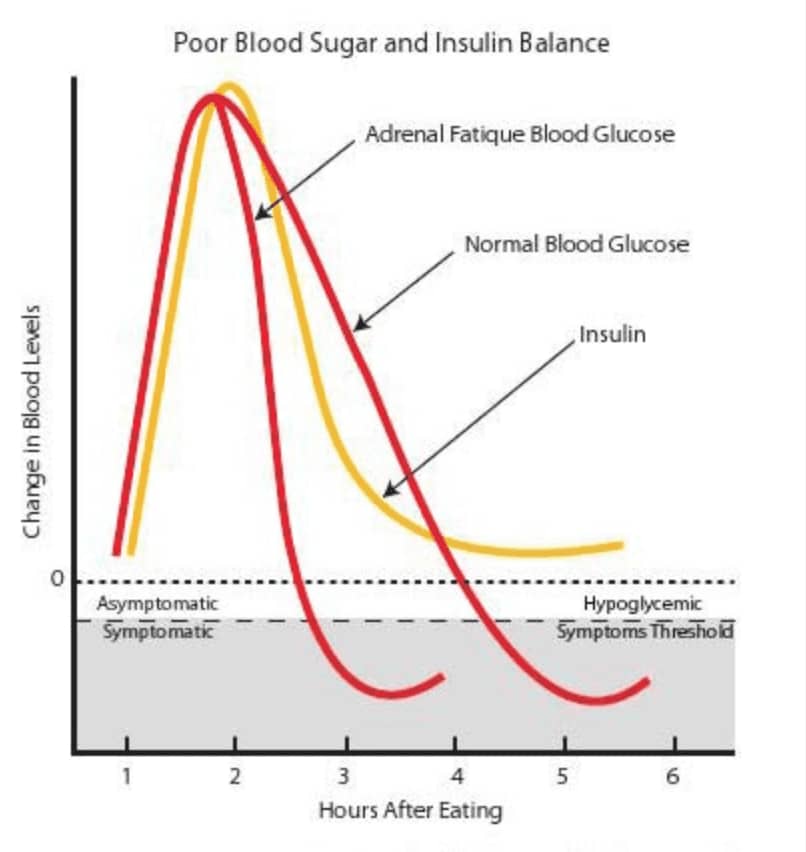
The diagram below shows how adrenal fatigue contributes to the symptoms of hypoglycemia. Compared to a normal person, or even someone with compromised insulin control, people with adrenal fatigue tend to have symptoms of hypoglycemia, even when blood glucose levels are within the normal range. This phenomenon is clinically evident.
After a meal, people with advanced adrenal fatigue tend to see their blood glucose levels fall below the hypoglycemic symptom threshold (HST) faster than normal. This triggers hypoglycemic symptoms such as irritability and fatigue. The more advanced the adrenal fatigue, the more the blood glucose curve is shifted to the left. As a result, the time between the end of a meal and the onset of hypoglycemia symptoms is shortened.
Adrenal exhaustion and sex hormone balance
Remember that when your adrenals have to constantly increase their production of cortisol, they eventually go haywire. This leads to adrenal fatigue syndrome (AFS).
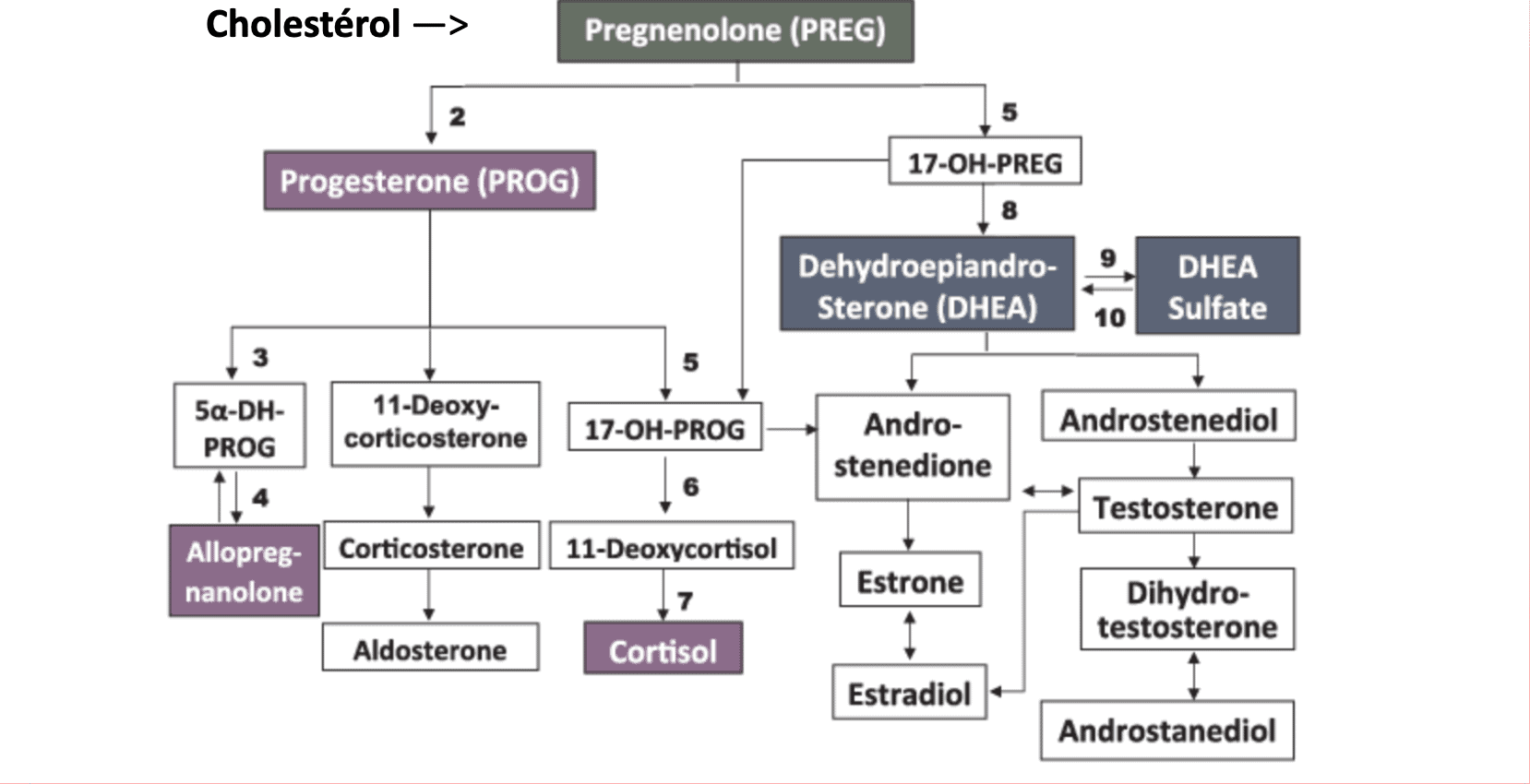
Following chronic stress, the pre-hormone (pregnenolone) is transformed into cortisol to the detriment of estrogen and testosterone production. It is therefore essential to regain an overall neuro-hormonal and metabolic balance by modulating stress in order to restore the balance of sex hormones.
Symptoms of adrenal exhaustion linked to an imbalance of sex hormones:
- Fatigue
- Weight gain
- Anxiety
- Mild depression
- Mental fog
- Premenstrual syndrome
- Infertility
- Decreased libido
- Reduced immunity
- Hypoglycemia
- Salt and sugar cravings
- Hair loss
- Dry skin
- Heart palpitations
The foundations of health
The hypotoxic, anti-inflammatory diet with fresh, organic superfoods
We can rebalance our neuro-hormonal systems by giving the body what it needs to produce neuro-hormones and avoid developing an inflammatory terrain. For a healthy nervous and hormonal system, we need lots of nutrients from a diversified, fresh and, if possible, organic diet: plenty of leafy green vegetables, nuts and seeds, good-quality proteins, nutrient-rich carbohydrates (whole quinoa, brown rice, millet, etc.) and healthy fats, including those found in oily fish.
Micronutrients needed by the neuro-hormonal system:
- Group B vitamins (or B complex) especially B6, B9 and B12
- Vitamin D
- Selenium
- Zinc
- Iodine
- Omega 3 and cholesterol from good fats (but mainly from liver synthesis)! monounsaturated (olive, avocado) and polyunsaturated (fish, flax) fatty acids
- Antioxidants (to protect these good fats): vitamins C, E and selenium
- Avoid pro-inflammatory foods: gluten-containing grains (wheat, barley, rye, oats), dairy products, reduce natural sugars (honey, maple syrup, cane sugar, molasses) and eliminate processed sugars (sucrose, sucrose, fructose) and simple carbohydrates (white bread and rice, mashed potatoes), processed, “prepared” or burnt foods (chips, French fries, caramel, barbecued meats, burnt toast).
NaturaMed offers optimal, personalized naturopathic dietary guidance (kinesiology) for neuro-endocrine-metabolic balance.
Slow, coordinated breathing exercises for neuro-hormonal balance
A unique feature of mind-body interventions such as Qi-gong, cardiac coherence and Mindfulness over typical low-to-moderate intensity exercises is the inclusion of slow, deep breathing in synchrony with slow exercise movements. Slow breathing is known to have a balancing effect on the autonomic nervous system via increased parasympathetic activation. Slow, deep breathing stimulates stretch-induced inhibitory signals and hyperpolarizes currents propagated in cells, resulting in synchronization of neural elements in the heart, lungs, limbic system and cortex.
Slow breathing also enhances vagal activity, leading to a reduction in psychophysiological arousal and a decrease in sympathetic activity and stress responses, and is associated with a reduction in the severity of symptoms of post-traumatic stress disorder (PTSD) or any chronic stress resulting from trauma.
There is an approach, Qi Conscience plein air ™ (Qi or Vital Energy, Mindfulness, Outdoor), which combines these approaches for a more effective and enjoyable neuro-hormonal connection! Workshops are given regularly by NaturaMed. Check out our upcoming activities in Events.


Recent Comments